Peng Min’s Team from Tsinghua University Reports Curative Cell Therapy for Asthma in Nature Immunology
Source:Peng Min
2024-06-18
Common chronic diseases are major threats to human health, affecting all organ systems, having high incidence rates, being unavoidable, and incurable, which leads to a heavy disease, economic, and social burden. Asthma is the most common respiratory disease, with over 300 million asthma patients worldwide and over 250,000 deaths annually due to severe asthma. Like other common chronic diseases, asthma is an incurable lifelong condition that requires lifelong treatment.
Type 2 inflammatory factors play a key pathogenic role in asthma. Using protein drugs to block Type 2 inflammatory factors has some efficacy in treating asthma and reduces the use of glucocorticoids. However, like traditional small-molecule drugs, protein drugs require long-term or even lifelong administration, can cause side effects after long-term use, and patients may develop antibodies against these proteins, leading to reduced efficacy. Therefore, the efficacy of protein drugs for asthma is limited; they cannot be used alone and cannot cure asthma. Chimeric antigen receptor T (CAR-T) cells, as living drugs, have the potential to cure chronic diseases due to their persistence in the body. Currently, CAR-T cells have achieved clinical cures in some B-cell leukemia patients, but whether CAR-T cells can cure non-tumor chronic diseases has no precedent.
On May 27, 2024, Peng Min's research team at Tsinghua University published a paper titled "A single infusion of engineered long-lived and multifunctional T cells confers durable remission of asthma in mice" in Nature Immunology. This study reports a curative therapy for asthma based on long-lived CAR-T cells, which achieves long-term efficacy in animal models with a single infusion, reaching a curative effect. This study is the first to achieve a cure for asthma, a common disease, in animal models using CAR-T cells, opening a new chapter for the use of cell therapy to cure common non-tumor diseases.
CAR-T cell therapy for non-tumor chronic diseases faces three major obstacles. First, the causes of most common chronic diseases are complex and irremovable (such as environment, aging, etc.), the condition is recurrent, and persists for life. This requires CAR-T cells used for treatment to have lifelong persistence, meaning a single infusion, lifelong existence, and lifelong effectiveness. Second, current CAR-T cell therapy requires patients to undergo chemotherapy-based pretreatment ("lymphodepletion"), which is unacceptable for non-tumor patients due to the severe side effects of chemotherapy. Third, unlike tumors, cells affected by chronic diseases (such as heart, liver, lung, kidney, brain, etc.) cannot be simply cleared by CAR-T cells because these tissues and organs have indispensable physiological functions. Therefore, selecting appropriate CAR-T targets is particularly important.
To address the issues of CAR-T cell persistence and chemotherapy pretreatment, Peng Min's team discovered a unique gene combination in the genome through whole-genome CRISPR screening, namely BCOR and ZC3H12A. Knocking out these two genes makes CAR-T cells enter a new state, termed "Immortal-like and Functional T cells" (TIF). CARTIF cells have the ability to self-renew indefinitely like induced pluripotent stem cells (iPSCs) and can exist in the body for life. Unlike iPSCs, CARTIF cells do not lose lineage characteristics and functions but retain the characteristics and physiological functions of mature T cells. The relevant research results were published in J Exp Med in May 2024.
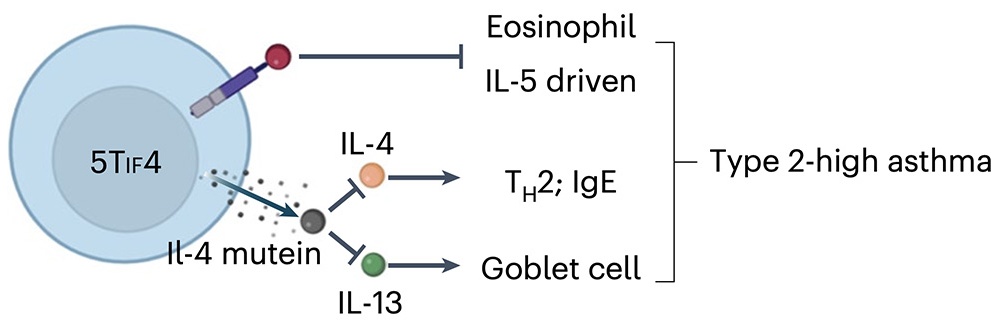
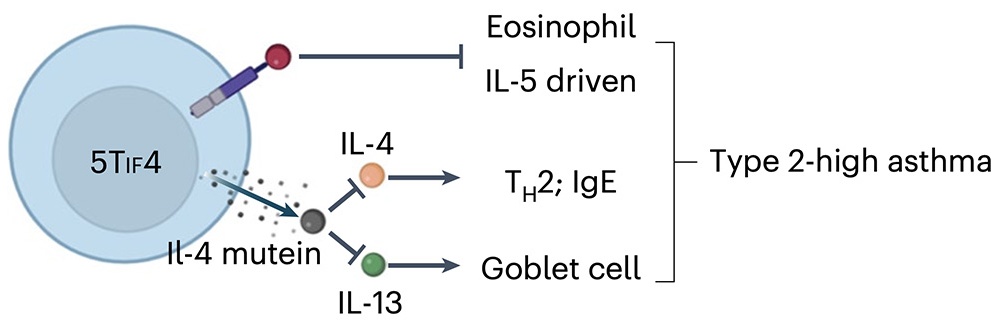
After solving the issues of CAR-T cell persistence and chemotherapy pretreatment, Peng Min's team applied the new concept and technology platform of CARTIF to the most common respiratory disease, asthma. The team constructed IL-5 CAR-T cells that recognize and kill eosinophils (which highly express the IL-5 receptor) by using IL-5 as the CAR's antigen-binding domain and inserted the TIF program into IL-5 CAR-T cells through gene editing. This allows the cells to proliferate and clear eosinophils in immunocompetent mice without any pretreatment. Additionally, the cells were further engineered to secrete a mutant IL-4 that inhibits both IL-4 and IL-13 long-term, named 5TIF4 cells. In various asthma models, a single infusion of 5TIF4 cells achieved long-term clearance of eosinophils and sustained inhibition of IL-4 and IL-13, significantly alleviating lung inflammation, eliminating asthma symptoms, and achieving a curative effect.
In summary, this study is the first to report a single-infusion curative cell therapy for asthma, providing a new approach and preclinical product for curing common respiratory diseases. In the future, this research is expected to bring an "once-and-for-all" therapy to hundreds of millions of asthma patients (especially those with severe asthma), rewriting the history of incurable chronic diseases.
Associate Professor Peng Min of Tsinghua University is the corresponding author of the paper, and team members Jin Gang and Liu Yanyan are the co-first authors of the paper. The research was supported by the National Natural Science Foundation of China, Tsinghua-Peking Center for Life Sciences, Tsinghua University, and Tsinghua University's Institute of Immunology.
Original links: https://www.nature.com/articles/s41590-024-01834-9
Review articles highlighting the research:
https://www.nature.com/articles/s41590-024-01851-8
https://www.nature.com/articles/s41577-024-01055-z
https://doi.org/10.1084/jem.20240258
Type 2 inflammatory factors play a key pathogenic role in asthma. Using protein drugs to block Type 2 inflammatory factors has some efficacy in treating asthma and reduces the use of glucocorticoids. However, like traditional small-molecule drugs, protein drugs require long-term or even lifelong administration, can cause side effects after long-term use, and patients may develop antibodies against these proteins, leading to reduced efficacy. Therefore, the efficacy of protein drugs for asthma is limited; they cannot be used alone and cannot cure asthma. Chimeric antigen receptor T (CAR-T) cells, as living drugs, have the potential to cure chronic diseases due to their persistence in the body. Currently, CAR-T cells have achieved clinical cures in some B-cell leukemia patients, but whether CAR-T cells can cure non-tumor chronic diseases has no precedent.
On May 27, 2024, Peng Min's research team at Tsinghua University published a paper titled "A single infusion of engineered long-lived and multifunctional T cells confers durable remission of asthma in mice" in Nature Immunology. This study reports a curative therapy for asthma based on long-lived CAR-T cells, which achieves long-term efficacy in animal models with a single infusion, reaching a curative effect. This study is the first to achieve a cure for asthma, a common disease, in animal models using CAR-T cells, opening a new chapter for the use of cell therapy to cure common non-tumor diseases.
CAR-T cell therapy for non-tumor chronic diseases faces three major obstacles. First, the causes of most common chronic diseases are complex and irremovable (such as environment, aging, etc.), the condition is recurrent, and persists for life. This requires CAR-T cells used for treatment to have lifelong persistence, meaning a single infusion, lifelong existence, and lifelong effectiveness. Second, current CAR-T cell therapy requires patients to undergo chemotherapy-based pretreatment ("lymphodepletion"), which is unacceptable for non-tumor patients due to the severe side effects of chemotherapy. Third, unlike tumors, cells affected by chronic diseases (such as heart, liver, lung, kidney, brain, etc.) cannot be simply cleared by CAR-T cells because these tissues and organs have indispensable physiological functions. Therefore, selecting appropriate CAR-T targets is particularly important.
To address the issues of CAR-T cell persistence and chemotherapy pretreatment, Peng Min's team discovered a unique gene combination in the genome through whole-genome CRISPR screening, namely BCOR and ZC3H12A. Knocking out these two genes makes CAR-T cells enter a new state, termed "Immortal-like and Functional T cells" (TIF). CARTIF cells have the ability to self-renew indefinitely like induced pluripotent stem cells (iPSCs) and can exist in the body for life. Unlike iPSCs, CARTIF cells do not lose lineage characteristics and functions but retain the characteristics and physiological functions of mature T cells. The relevant research results were published in J Exp Med in May 2024.
After solving the issues of CAR-T cell persistence and chemotherapy pretreatment, Peng Min's team applied the new concept and technology platform of CARTIF to the most common respiratory disease, asthma. The team constructed IL-5 CAR-T cells that recognize and kill eosinophils (which highly express the IL-5 receptor) by using IL-5 as the CAR's antigen-binding domain and inserted the TIF program into IL-5 CAR-T cells through gene editing. This allows the cells to proliferate and clear eosinophils in immunocompetent mice without any pretreatment. Additionally, the cells were further engineered to secrete a mutant IL-4 that inhibits both IL-4 and IL-13 long-term, named 5TIF4 cells. In various asthma models, a single infusion of 5TIF4 cells achieved long-term clearance of eosinophils and sustained inhibition of IL-4 and IL-13, significantly alleviating lung inflammation, eliminating asthma symptoms, and achieving a curative effect.
In summary, this study is the first to report a single-infusion curative cell therapy for asthma, providing a new approach and preclinical product for curing common respiratory diseases. In the future, this research is expected to bring an "once-and-for-all" therapy to hundreds of millions of asthma patients (especially those with severe asthma), rewriting the history of incurable chronic diseases.
Associate Professor Peng Min of Tsinghua University is the corresponding author of the paper, and team members Jin Gang and Liu Yanyan are the co-first authors of the paper. The research was supported by the National Natural Science Foundation of China, Tsinghua-Peking Center for Life Sciences, Tsinghua University, and Tsinghua University's Institute of Immunology.
Original links: https://www.nature.com/articles/s41590-024-01834-9
Review articles highlighting the research:
https://www.nature.com/articles/s41590-024-01851-8
https://www.nature.com/articles/s41577-024-01055-z
https://doi.org/10.1084/jem.20240258


